Stay Awesome

Keeping up to date: Things to know in practice currently:
Jan 2026: From Valneva: New downloadable content. There are three videos for your digital displays: Chikungunya map, Japanese Encephalitis Map and a Mosquito-borne disease video.
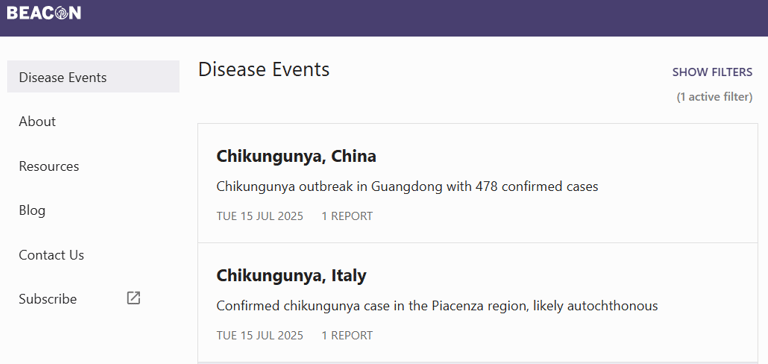
2025 has seen an increase in chikungunya cases in the UK. 73 cases were reported between January and June 2025, compared with 27 cases during the same period in 2024. Chikungunya cases have been reported in forty different countries in 2025, including France, Italy, India, China, Thailand, and Indonesia
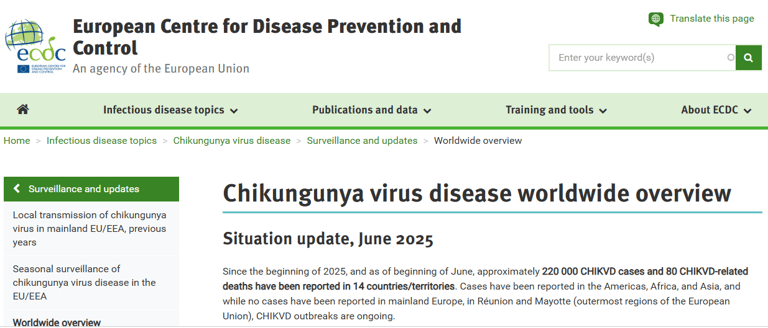
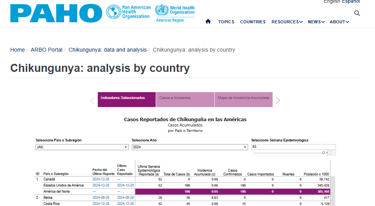
3rd October 2025: The WHO published an update on the current global situation of chikungunya virus (CHIKV) disease. Between 1 January and 30 September 2025, a total of 445,271 suspected and confirmed cases of CHIKV (155 deaths) were reported globally. So far in 2025, the region of the Americas has reported the highest number of cases.
15th October: Locally acquired chikungunya reported in New York state, first US case in 6 years
1st October: Valneva reports good antibody persistence for chikungunya vaccine. Data from 254 healthy adults suggested that 95% retained an antibody response above the seroresponse threshold for 4 years after a single dose. Antibody persistence in adults age 65 and older was similar to that for younger adults
25th August: Valneva Announces FDA’s Decision to Suspend License of Chikungunya Vaccine IXCHIQ In the U.S. Ominous sounding news?...
14th August: News Article from UKHSA: Rise in chikungunya cases in UK travellers returning from abroad. There have been 70 cases of chikungunya in the first six months of this year. This is more than double the number of cases compared to the same period in 2024.
7th August: FDA tightens label of Valneva's chikungunya vaccine, lifts pause in older adults
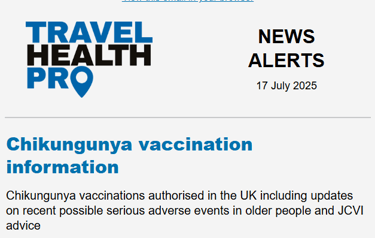
25th July: NaTHNAC have updated their news and now CHIK has made it's way to the vaccine recommendation lists. Also note this new information about chikungunya risk assessment.
19th June 2025: BMJ article: UK pauses chikungunya vaccine (IXCHIQ) in over 65s to conduct safety review. Ironic (and perhaps not a coincidence given it's live?) that the population advised not to use IXCHIQ vaccine are those individuals who are more at risk from developing severe chikungunya disease... There are currently no concerns with the use of the vaccine-like particle vaccine, Vimkunya, in adults over the age of 65 years, so could this be the preferred option for those older travellers for the time being? Although limited data there too in that age group.
9th June 2025: Chikungunya vaccine (IXCHIQ) temporarily paused in people aged 65 and over as precautionary measure while the MHRA conducts the safety review. As of 02 May 2025, 19 cases of serious adverse events (SAEs) following vaccination with IXCHIQ have been reported worldwide, thereof 12 from France and 6 from the United States and 1 from Austria. Many of the patients affected also had other illnesses and the exact cause of these adverse events and their relationship with the vaccine have not yet been determined. So far, 17 serious cases involved vaccinated individuals aged between 62 and 89 years, two of which resulted in death. As a temporary measure, while a thorough assessment of all available data is performed, IXCHIQ must not be used in adults aged 65 years and above. IXCHIQ can continue to be used in people aged 18-64 years, in accordance with official recommendations. Of course, remember the other contraindications too: IXCHIQ is contraindicated in immunodeficient or immunosuppressed individuals due to disease or medical therapy, independent of age.
14th May 2025: Worth a read of NaTHNaC's perspective on the recent adverse events data...
and here is the USA approach to it. "Suspend Use of Live Attenuated Chikungunya Vaccine in Adults Aged 60+, Agencies Advise"
7th May 2025: Announcement from Valneva following an EMA announcement on use of IXCHIQ in the older age groups. EMA has suspended the use of the vaccine for individuals over 65 years old but has maintained current recommendations for IXCHIQ for people from 12 to 64 years of age.
1st May 2025: A second Chik vaccine approved by MHRA!!! Vimkunya vaccine approved to prevent disease caused by the chikungunya virus in people 12 years of age and older
April 2025: French health authorities suspend use of Valneva's chikungunya vaccine in older adults to probe 3 hospitalizations, one death
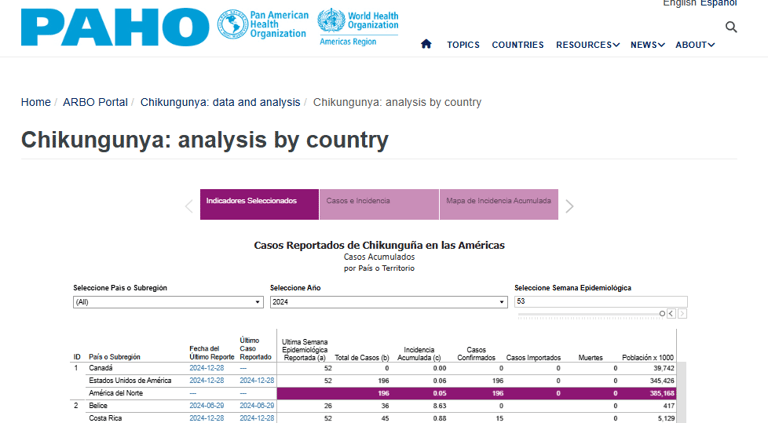
14th April 2025: Brazil authorises Valneva’s chikungunya vaccine (marking the first approval of a chikungunya vaccine in an endemic country- YAY!). Brazil has been the hardest hit country in the Americas, recording more than 1 million cases between January 2019 and July 2024. Definitely needed and will further open up more data and trial possibilities.
21st March 2025: Chikungunya wave hits Sri Lanka
27th Feb 2025: CDC investigating hospitalizations of five people who recently received chikungunya vaccine
4th Feb 2025: IXCHIQ has a UK licence!

Vimkunya (Bavarian Nordic) – MHRA approved May 1, 2025 for individuals aged 12+
Recombinant virus-like particle (VLP) vaccine—single 0.8 mL dose, IM injection
Seroresponse rates up to 98 % in 12–64 yrs; ~87 % in ≥ 65 yrs at 3 weeks, ~76–86 % at 6 months
Common reactions: injection site pain, fatigue, headache, myalgia
Scheduling: Give ≥ 2 weeks before travel when possible
Ixchiq (Valneva)
Live-attenuated vaccine, approved in Feb 2025 for individuals 18+
Single dose 0.5ml IM; initial seroresponse ~99%, remains high at 3 years in younger adults
Caution: temporarily restricted in people ≥ 60/65 yrs due to serious adverse events reported globally. Valneva notice here with more details.


JCVI Advice:
Vimkunya may be offered for those aged ≥ 12 traveling to outbreak areas or lab workers
Ixchiq may be offered to healthy individuals aged 18–59 if live vaccine is appropriate—avoid in ≥ 60yrs for now (see alerts above). Also careful with thymus dysfunction history!
Want to geek out? Go deeper here:
11th June: Chikungunya vaccine could stop millions of infections worldwide, study finds
4th June 2025: Chikungunya: All You Need to Know About Virus Spreading in Mombasa
30th April 2025: Interesting blog by my good friend and colleague Michelle Hunter. What Do We Know About The New Chikungunya Vaccine So Far?
23rd July 2025: Chikungunya virus disease returns to Europe: a turning point for the global arboviral landscape
30th July: WHO warns of global chikungunya threat as outbreak grows
8th August: check out the enticing title of this article.... China deploys ‘cannibal’ mosquitoes and killer fish to fight chikungunya.
Valneva have created a fabulous training resource for travel healthers "Neva". Lots of useful modules on there including a lovely NEW one all about Chikungunya. Free to register - and well worth it! click the picture below. Also order some resources - click the other link for those!


What is chikungunya anyway?
Chikungunya is a viral infection caused by Chikungunya virus, transmitted via Aedes mosquitoes. It causes sudden high fever and severe joint pain—symptoms that can linger for weeks or even months. The word “chikungunya” comes from a term meaning “that which bends up,” referring to the posture forced by joint pain. Chikungunya is an alphavirus with three genetically distinct lineages which was first identified as a result of a significant outbreak in southern Tanzania in 1952.
What happens If you catch it?
Symptoms typically appear 4–8 days after a bite and include high fever, debilitating polyarthralgia (usually in hands and feet), headache, rash, and fatigue. Though mortality is rare, persistent joint pain and fatigue can significantly impact quality of life—especially in older adults.
How does It Spread?
Via bites from Aedes aegypti or Aedes albopictus, daytime mosquitoes found in many tropical, subtropical, and increasingly, Mediterranean regions. Mosquitoes become infected when they feed on viremic nonhuman or human primates, both of which are likely the main amplifying reservoirs of the virus. Humans are typically viremic shortly before and in the first 2–6 days of illness. Bloodborne transmission is possible; 1 case has been documented in a health care worker who sustained a needle stick after drawing blood from an infected patient. Furthermore, chikungunya virus has been identified in donated blood products undergoing screening, although no transfusion-associated cases have been identified to date. Maternal–fetal transmission has been documented during pregnancy; the greatest risk occurs in the perinatal period when the pregnant woman is viremic at the time of delivery. Although chikungunya viral RNA was identified in the breast milk of 1 infected person, the breastfed infant had no symptoms or evidence of infection based on laboratory testing. Additionally, chikungunya viral RNA has been identified in semen, but no evidence of sexual transmission has been noted to date.
Does getting chikungunya make you Immune?
Yes—natural infection usually confers lifelong immunity. Vaccination induces protective immunity safely, without disease.
Can it be treated?
No specific antiviral. Treatment is supportive: fluids, rest, and non-steroidal anti‑inflammatory drugs. Severe or prolonged symptoms may warrant rheumatology referral or physical therapy.
Who’s most at risk?
Travellers to regions experiencing chikungunya outbreaks
Longer-stay visitors to Asia, Africa, the Americas, or Southern Europe (by the way, England may become a suitable habitat for the Aedes mosquitoes by the 2040s/2050s.)
Older adults (more likely to have chronic arthritis post-infection)
People with pre-existing joint conditions
Laboratory staff working with chikungunya virus

Top reasons to encourage vaccination (when indicated):
In the first quarter of 2025, ~80,000 cases and 46 chikungunya related deaths in 14 countries/territories were reported. The highest burden of disease has been seen in Brazil, with high levels also seen in La Réunion and Mayotte.
Vaccines are now licensed in the UK
It’s very common in travellers. In one study, chikungunya was the second most common cause of fever in returned travellers from the Indian Ocean and Caribbean regions, just behind dengue (GeoSentinel data, 2016).
Prevents a painful, disabling illness: Severe joint pain affects up to 90% of symptomatic cases—and it can last for months or years. It’s not just “a bit of a virus.”
No treatment exists. The only protection is prevention.
Older adults are more likely to have long-term symptoms. Around 30–40% of those aged over 45 report pain 3–12 months after infection.
Outbreaks can occur in popular holiday hotspots like Mauritius, Thailand, Brazil, and southern Europe (Italy, France). Travellers may be unaware they’re heading into an active zone.
A single bite can infect! Aedes mosquitoes bite during the day and often indoors—repellent is helpful but not foolproof.
Hospitalisation may be needed in 5–8% of cases, even in healthy people. In high-risk groups (older adults, those with chronic disease), severe illness is more likely.
Mortality is low but real—up to 1 in 1,000 symptomatic cases die during outbreaks in older or immunocompromised populations.
Both Vimkunya and Ixchiq show strong antibody responses within 2–3 weeks of a single dose.
Better safe than sore. Yes, the vaccine can lead to a bit of an achy arm BUT travellers with prior joint issues, autoimmune disease, or fibromyalgia may experience months of flare-ups after infection with the disease. Vaccination is a much less achy option.
It ticks a gap in standard travel vaccines. Unlike shistosomiasis, Zika, or West Nile—which we are not fortunate enough to have vaccines for (yet...).