Stay Awesome

Keeping up to date: Things to know in practice currently:
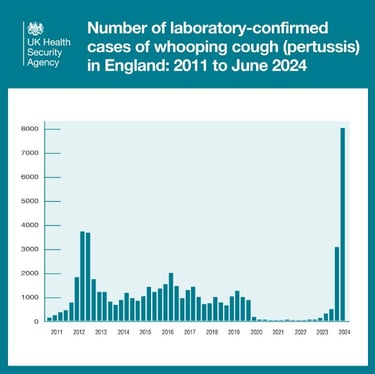
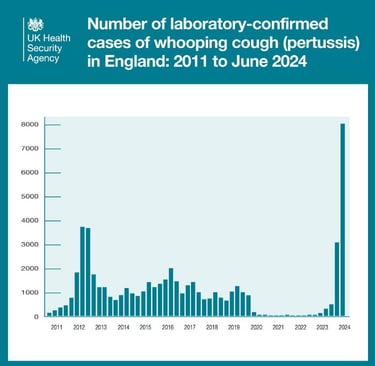
22nd Dec: Laboratory confirmed cases of pertussis in England: annual report for 2024 is in. In England, there were 14,879 new laboratory confirmed cases of pertussis in 2024. The number of cases in 2024 were the highest reported since 1994. There were 11 reported infant deaths from pertussis between January and December 2024. The 14,879 confirmed cases in England in 2024 were substantially higher than the 857 cases reported in 2023 and 58.8% higher than the last major outbreak in 2012 when 9,367 cases were reported. Thankfully, vaccination coverage seems to be steadily improving.
19th Dec: Latest figures show strong uptake of whooping cough vaccine in pregnancy. And this data in the news item came from this report.
19th Dec: The Green Book chapter was updated today too to align with published guidance on occupational pertussis vaccination of healthcare workers. HCWs who have not received a pertussis-containing vaccine in the last 5 years and have regular contact with pregnant women or young infants (defined as those under 3 months of age) are prioritised for occupational vaccination (with Boostrix, ADACEL or REPEVAX). There are two priority groups which are outlined in more detail in the GB, and there is a document linked within the Green Book but unfortunately the link was broken when I tried it.
17th Dec: Hexavalent combination vaccine: information for healthcare practitioners document was updated to include new training slides for download and updates to the main guidance document to reflect the introduction of MMRV to the routine schedule for children from 1 January 2026.
3rd Dec: This is such promising news about a new nasal vaccine for pertussis.
27th November: The data is now in for last year around pertussis cases and vaccine coverage. In England, there were 14,879 new laboratory confirmed cases of pertussis in 2024. The number of laboratory-confirmed cases in 2024 were the highest reported since the introduction of the Pertussis Enhanced Surveillance Programme in 1994. There were sadly, 11 reported deaths in infants who developed pertussis between January and December 2024. This is pretty significant considering there were no reported deaths in infants with confirmed pertussis between 2020 and 2022, and only one death reported in 2023. All the deaths following the introduction of the prenatal programme to end December 2024, occurred in infants who were too young to be fully protected by their primary vaccinations, some with co-infections and/or underlying health complications. Of the 32 infants that have died since the introduction of the vaccine, 26 were born to mothers who were not vaccinated in pregnancy. Estimated vaccine effectiveness against death in infants with pertussis whose mothers had been vaccinated, including recent deaths to the end of August 2024, is estimated to be very high at around 91%. Also worth noting that 8 deaths occurred last year in adults over 65.
Vaccine coverage estimates for 2024/2025 financial year, evaluated between April 2024 to March 2025 for DTaP/IPV/Hib/HepB immunisation across England, was 91.3% for 3 doses at 12 months of age and 81.3% for the booster dose by 5 years of age. And in the prenatal groups fortunately, following a substantial decline during the pandemic period, substantial improvements in prenatal coverage were seen over the course of 2024 nationally, with this trend to increasing coverage seen across all regions nationwide. Monthly uptake ranged from 58.9% to 68.2% across the year. Coverage up to June 2025 was 70.2%.
The UKHSA stockholding of Vaxelis has depleted. Infanrix hexa is now the only DTaP/IPV/Hib/HepB vaccine available to order by ImmForm.
2nd October: PGD template updated for dTaP/IPV. The changes are mostly aesthetic and branding/consistency or referencing related, but also note they have added facilities for management of anaphylaxis, syncope, and those living with HIV in cautions section as per SPCs. And there is an addition of a statement regarding absence of reliable history for routine immunisation in dose and frequency section. They have amended criteria for inclusion and doses and frequency sections stating pertussis outbreaks in nurseries/schools to contacts and cases as per the guidelines, and clarified the section for management of tetanus prone wounds. Also updated is the storage conditions as per SPCs and added signposting to accessible information in written information provided.
25th September 2025: Vaccine coverage statistics are in for uptake on the maternal programme. Coverage was 72.2% in April 2025, 71.2% in May 2025 and 70.2% in June 2025. Quite an improvement from this time last year.
31st August 2025: Baby dies of whooping cough after mother not vaccinated while pregnant. Another poignant reminder of the importance of the maternal programme for young babies. Another baby whose mother was not vaccinated against whooping cough while pregnant has died after contracting the infection
26th June 2025: New figures released today in the vaccine uptake data by UKHSA show a significant and sustained increase in the number of pregnant women coming forward for the whooping cough vaccine. YAY!!! The latest data reveals a consistent seven-month upward trend in maternal pertussis vaccination rates. The rates climbed from 59.0% in May 2024 to nearly 73% in March this year. Uptake rates are now almost as high as the peak at the start of the programme.
10th June 2025: The Pertussis Green Book chapter has been updated So has the PGD template for Hexavalent vaccine DTaP/IPV/Hib/HepB.
2nd June 2025: This guidance got an update: "Hexavalent DTaP/IPV/Hib/HepB combination vaccine: information for healthcare practitioners". As did this page (Hexavalent combination vaccine: programme guidance) in general.
29th May 2025: More resources - an updated slideset for the hexavalent programme. To help with understanding the changes in the programme from July 2025.
24th April 2025: Quarterly pertussis vaccine coverage data released. Pleasing to see that coverage has consistently increased over the preceding 8 months although still hovering around the 68% uptake mark. So, onwards and upwards!

Reminders:
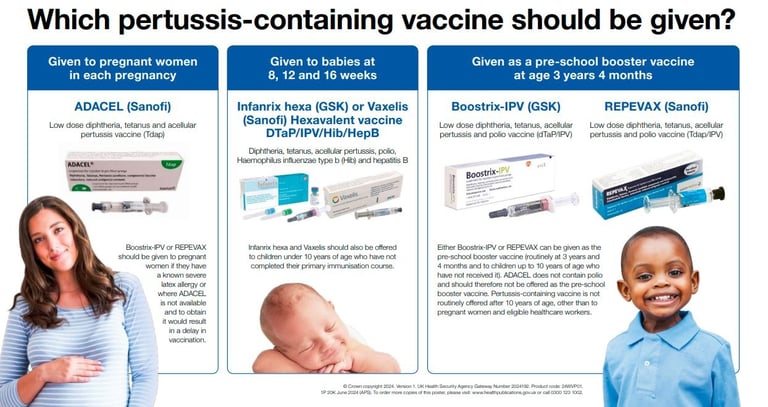
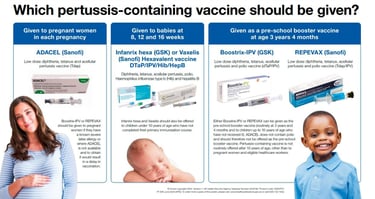
Acellular vaccine, part of DTaP/IPV and Tdap/IPV
Maternal dose 16 weeks+ of pregnancy
UK childhood schedule (Infanrix/Vaxellis): 2, 3, 4 months, 18m (DOB depending) + 3y 4m booster
Repevax is current UK childhood brand (was Boostrix-IPV prior to Jan 2025). Adacel for pregnant ladies from July 2024 (due to not containing polio but the others can be given for example if allergies to the others OR if polio indicated e.g. for travel or outbreaks). See letter for more info.
Store at 2–8°C; IM injection
Have YOU checked your own vaccine status as a HCP?
Want to geek out? Go deeper here:
7th April 2025: New antibody research sparks hope for better whooping cough vaccines
4th Dec 2024: Intranasal pertussis vaccine? BPZE1 is designed to overcome deficiencies of current pertussis vaccines, including poor durability of protection and failure to prevent nasopharyngeal B. pertussis colonisation that leads to escape mutants and transmission to vulnerable infants. Looks set to be entering phase 3 trials in 2025...
This article about Pertussis uptake was published in the BMJ on 29th August 2024. Here's an extract that forms a good reflection opportunity: "Ongoing analysis of data from England shows that whooping cough vaccine, when given at the right time in pregnancy, provides 92% protection against infant death. Yet its uptake in England, from a high of 72.6% in March 2017, has now declined to 58.9%". We MUST get this higher!!!
Useful and informative TOP TIPS article from July 2024 emphasising some key points about Pertussis vaccination and also management of the disease.

What is pertussis anyway?
Caused by Bordetella pertussis, this highly contagious bacterial infection leads to intense coughing fits. It’s especially dangerous in babies and can cause pneumonia, seizures, and death. In 2018, there were more than 151 000 cases of pertussis globally.
What happens If you catch it?
Starts like a cold, then progresses to severe bouts of coughing (often with a “whoop” sound). Vomiting after coughing is common. Illness can last weeks to months—“the 100-day cough.” Some babies who get pertussis won’t cough at all. Instead, they will simply stop breathing or suffer with apnoea spells.
How does It Spread?
Airborne droplets from coughing or sneezing. Easily passed between close contacts. People with pertussis are most contagious up to about 3 weeks after the cough begins,
Does getting pertussis make you Immune?
Not for long. Immunity from infection or vaccination wanes over time—boosters are essential to maintain protection.
Can it be treated?
Yes—antibiotics (usually macrolides) can shorten infectious period, especially if started early. Supportive care for infants often involves hospitalisation.
Who’s most at risk?
Infants under 6 months (especially before primary doses), pregnant people, healthcare workers and carers of young babies, and adolescents and adults with waning immunity. The disease is most dangerous in infants under 3 months old, and is a significant cause of disease and death in this age group.

Top reasons to encourage vaccination (when indicated):
Prevents infant hospitalisation and death
Part of UK maternal and childhood schedule
Boosters protect adults and reduce spread to babies
Protect vulnerable patients: Required in many healthcare roles
Since the introduction of pertussis vaccination in pregnancy, from 2013 to the end of June 2024, there have been 30 deaths in babies with confirmed pertussis who were all too young to be fully protected by infant vaccination. Sadly, this includes the 9 deaths in infants who had contracted pertussis between January and July 2024. Of the 30 infants that died, 24 had mothers who were not vaccinated in pregnancy.
On the 8th August 2024 a 10th Baby died of pertussis in the UK. Also born to an unvaccinated mother. 10,000 cases had been reported at this point since the outbreak that began in November 2023 (although due to under-reporting is probably WAY higher). So sad.