Stay Awesome

A Scenario
Meet the Adeyemi family!! They are here to guide you through examples that occur in many types of practice. This page ends with lots of tips for practice so keep scrolling!
Grandmother – Grace Adeyemi (72)
Moved from Nigeria to the UK in her mid-20s in the early 1970s. Worked as an NHS nurse until retirement. Can't recall if she had occupational vaccines at any point and has no records of any. Lives with type 2 diabetes and hypertension.
Father – Daniel Adeyemi (45)
Born in the UK after Grace settled there. Works as a phlebotomist in an outpatient clinic. Childhood included extended trips back to Nigeria, leading to patchy vaccination records. Has mild asthma. Was not happy with Aisha's decision to decline flu vaccines for the kids this year.
Mother – Aisha Khan (39)
Born and raised in the UK, works part-time as an SEN teaching assistant. Loves cycling and baking. Generally proactive with her children’s health but sometimes anxious about vaccine safety after things she reads on social media. Declined flu vaccines for the kids this year due to a facebook comment about gelatin in vaccines.
Daughter – Samira Adeyemi (15)
Confident, active on TikTok, plays football. Missed some school immunisations when off sick, not yet caught up. Sometimes questions authority, influenced by peers/social media. Recently discovered veganism and feels very strongly about it. Adores animals.
Son – Yusuf Adeyemi (8)
In Year 4, keen on Minecraft and gaming. Gives a lot of high fives. Does not agree with early nights. Won't touch or even look at vegetables. Strokes every dog he sees- but usually Samira gets there first. Once got bitten on the ear by a dog in Pakistan when he was 5. No professional advice was sought at the time. Family isn’t entirely sure his vaccine records are complete due to multiple overseas visits when younger.
Baby Layla (9m)
Attends nursery three days a week. Enjoys chewing on things and pulling the cats tail. Raises strong objections to being injected. Some vaccines were delayed due to parents not knowing they were due.
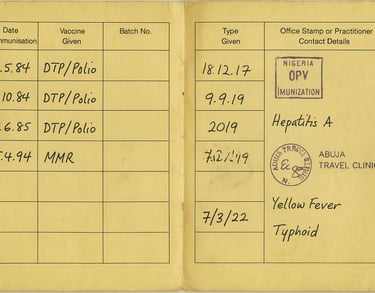
Graces vaccine records (very patchy!)
Get some practice with the UK routine schedule and the incomplete immunisation algorithm and see if you can devise a vaccine plan for her to align with the UK schedule.
Grace, remember, is 72, and living with T2 diabetes and hypertension. Let's assume it is the month of October currently.
What is she due and when?
Of these, which ones can you personally give and which ones will you refer to another health care professional?
What legal mechanism/s would you need in place to be able to administer them?
Travel healthers:
Grace is heading back to Nigeria to visit family in one month. She will be staying with friends, city based in Lagos and staying for 5 weeks.
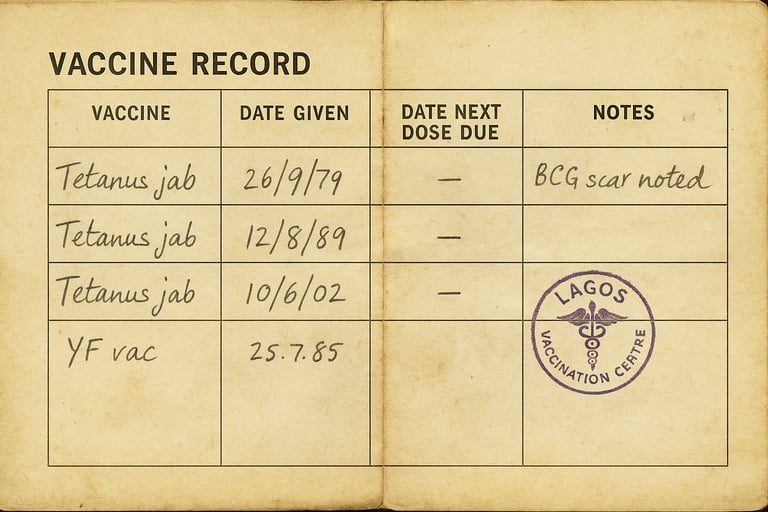
Using the NaTHNaC website, what will you advise her to get or consider? Of these, which ones can you personally give and which ones will you refer to another health care professional? What other advice will she benefit from? Will she need antimalarials? Are there any factsheets on there that you can give to her? HINT: this might be one of them. Can you find any others?
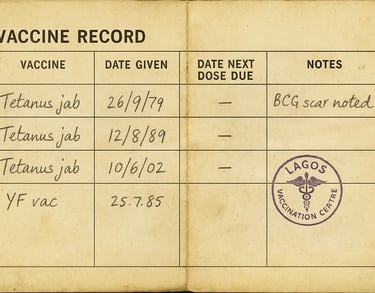
Daniels vaccine records
Get some more practice with the UK routine schedule and the incomplete immunisation algorithm and see if you can devise a vaccine plan for him to align with the UK schedule.
Daniel is 45 and living with asthma. Let's assume it is the month of October currently.
What is he due and when?
Of these, which ones can you personally give and which ones will you refer to another health care professional?
What legal mechanism/s would you need in place to be able to administer the ones you will give?
Food for thought: Are there any vaccines that might need consideration about their intervals given the family travel plans? If you are unsure take a look at the end of ch 11 of the Green Book)
Travel healthers: Daniel is accompanying Grace on the Nigeria trip in one month. He's staying for 5 weeks too. Using the NaTHNaC website, what will you advise him to get or consider? Of these, which ones can you personally give and which ones will you refer to another health care professional? What other advice will he benefit from? Will he need antimalarials? Are there any factsheets on there that you can give to him? HINT: this might be one of them.
Occupational healthers: Daniel woks part time as a phlebotomist in a hospital setting currently and is also studying a BSc at the local university to become a registered nurse, which requires lots of clinical placements. What vaccines might you suggest he requires here and how would you approach this from a scheduling perspective?
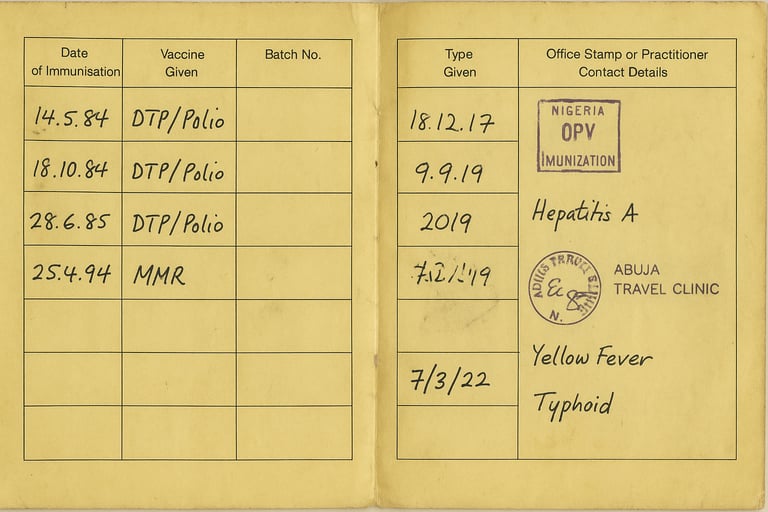
Aishas vaccine records
Get yet more practice with the UK routine schedule and the incomplete immunisation algorithm and see if you can devise a vaccine plan for her to align with the UK schedule.
Aisha is 39, and has no medical conditions but here's a curveball - she is 24 weeks pregnant. Let's assume it is the month of October currently.
What is she due and when?
Of these, which ones can you personally give and which ones will you refer to another health care professional?
What legal mechanism/s would you need in place to be able to administer them?
Travel healthers:
Aisha has decided not to accompany the others to Nigeria this time due to her pregnancy and Layla being so young, but may still be susceptible to changing her mind.
Using the NaTHNaC pregnancy factsheet and the travel with children factsheet, consider what risk factors may have led to this decision in order to help support her decision.


Samiras vaccine records
Get yet more practice with the UK routine schedule and the incomplete immunisation algorithm and see if you can devise a vaccine plan for her to align with the UK schedule.
Samira is 15, and has no medical conditions. Let's assume it is the month of October currently.
What is she due and when?
Of these, which ones can you personally give and which ones will you refer to another health care professional?
What legal mechanism/s would you need in place to be able to administer them?


Travel healthers:
Samira is the only one of the children going on the Nigeria trip with Grace and Daniel. She has visited Pakistan but never been to Nigeria before.
Using the NaTHNaC website, what will you advise her to get or consider? Of these, which ones can you personally give and which ones will you refer to another health care professional? What other advice will she benefit from? Will she need antimalarials? Are there any factsheets on there that you can give to her? HINT: this might be one of them. Can you find any others? Here's an interesting piece of information that's quite relevant here: 40 percent of rabies cases are in children under 15 years of age... And THIS is something important to have on the radar too.
Yusufs vaccine records
Get even more practice with the UK routine schedule and the incomplete immunisation algorithm and see if you can devise a vaccine plan for him to align with the UK schedule.
Yusuf is 8 and medically well. Let's assume it is the month of October currently. He is not going on the trip to Nigeria but has been to Pakistan a few times in the past.
What is he due and when?
Of these, which ones can you personally give and which ones will you refer to another health care professional?
What legal mechanism/s would you need in place to be able to administer the ones you will give?
Why might Yusuf have oral polio vaccinations in his records? This factsheet will help you to find the answer.
VERY IMPORTANT: How would you approiach the dog bite he sustained in Pakistan when he was 5? This guidance will take you through it. Whatever area of practice you are in and whatever job title you have, this needs to be escalated!!!


Layla's vaccine records
I bet you're exhausted now!! Well done for getting this far. LAST one (well, for this family scenario) I promise!
Use the UK routine schedule and the incomplete immunisation algorithm to devise a vaccine plan for Layla to align with the UK schedule.
Remember, she is 9 months old and medically well. Let's assume it is the month of October in the year 2025 currently.
What is she due and when?
Of these, which ones can you personally give and which ones will you refer to another health care professional?
What legal mechanism/s would you need in place to be able to administer the ones you will give?
After this appointment, when if her next one and what will she receive then?
How will you make sure no more future appointments are forgotten by the parents?


Let's bring this back to YOU and your clinic for some reflection.
Some of these scenarios relate to identifying and linking up with other professionals who might be delivering different vaccines to your area of practice. As we have seen in those examples above, sometimes GP's are the ones to go to, other times maternity services are responsible, sometimes occupational health, school health, travel health or sexual health should be taking the reigns.
REFLECT NOW: In your practice what do you do to:
Highlight the necessity of vaccines in general?
Aid with signposting to the right places when you don’t provide the immunisation in question?
Link up with other organisations so they know you exist (and you know they exist) if a vaccine need comes up?
Determine eligibility?
Integrate vaccines into other appointments and reviews?
Diabetes review? Have a check.
Travel heath appointment in a private clinic? Get the NHS schedule out.
COVID or Flu mass vaccination clinic? Don't forget to mention any others due.
Occupational health appointment? Start with addressing the national schedule.
Midwife appointment or home visit as a health visitor? Prep that parent. Get some immunisation information in there.
Sexual health appointment for mpox or gonorrhoea vaccines? Check them all!
Check check check!! And refer if necessary.
All of the Adeyemi family scenarios relate to missed vaccines and incomplete schedules. Think about WHY they might have ended up in this situation. How did they get missed? REFLECT NOW: What can YOU do to ensure your clientele do not miss the vaccines they will benefit from (whether you are the one giving them or not!)?
These tips might help.
Have a look at the NICE guidance for increasing uptake. How do you follow up on low-uptake vaccines and those who decline or miss appointments?
Make it a monthly task to determine your eligible patients
Nominate a dedicated ‘disease’ lead for low uptake vaccines or high volume programmes (e.g. flu, shingles)
Prioritise your immunocompromised patients for those vaccines that are for higher risk populations. Shingles uptake, for example, is generally much lower in the immune-compromised group compared to the age-based groups.
Encourage next-dose compliance - for example ensure at each appointment that person knows when to expect the next one and advise they diarise it too. Give written and electronic reminders and ensure they are all set or automated at the current appointment.
Educate EVERYONE at work!! Reception teams included. The NHS plan encourages educating ALL staff who might have vaccine discussions. This include reception teams and other non-clinical staff.
Raise awareness. Make vaccinations visible and important in your area of practice. Have leaflets and posters visible in the waiting room and on your website. Have a good browse of the NHS publications website which has loads of free stuff to order, and browse vaccine manufacture sites as well - they often have free materials too, like vaccine record books and disease-specific posters and leaflets. For general immunisation promotional resources go to this page. And for travel healthers also look at this page for ideas.
Give more information with your invites so people understand the importance of attending.
Run dedicated vaccine clinics such as 'Shingles mornings' or 'childhood catch ups'.
Don't forget - this is PERSONAL too! Check in on your eligible friends and relatives. You know how to work things out if you just completed these scenarios!
Opportunistically check on those who could be eligible. Make every visit count (as above)! Set alerts. Code and flag.
Birthday cards! Invite as soon as people become eligible if it is an age-based programme such as RSV, Shingles, flu...
Don’t forget the housebound patients – make provision.
Let's address Aisha's vaccine hesitance and the missed flu vaccines for the children.
How can YOU increase vaccine confidence?
Can you make use of these resources and tips on this page to to better inform people?
My personal favourite websites to promote public knowledge and confidence are those of the vaccine knowledge project and Jitsuvax. Have a good browse!